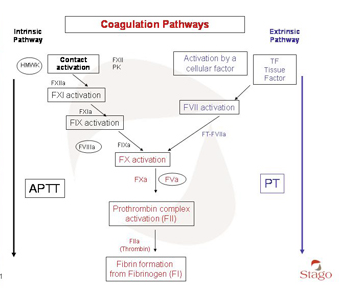
Figure 1 = coagulation cascade
Lengthening of Quick's time and activated partial thromboplastin time and factor deficiencies
Lengthening of Quick's time occurs in the event of a deficiency of factor I (fibrinogen), factor II (prothrombin), factor V (proconvertin), factor VII (proaccelerin) or factor X (Stuart factor).
Lengthening of activated partial thromboplastin time indicates deficiency of factor I (fibrinogen), factor II (prothrombin), factor V (proconvertin), factor X (Stuart factor), factor VIII (antihaemophilic factor A), factor IX (antihaemophilic factor B), factor XI (Rosenthal factor) or factor XII (Hageman factor).
Lengthening is dependent upon the sensitivity of the reagent to deficiencies in the factors concerned. Furthermore, certain reagents used to determine activated partial thromboplastin time may also allow detection of deficiency of two factors involved in the contact phase of coagulation, prekallikrein (Fletcher factor) and high-molecular-weight kininogen, deficiencies of which are rare and not clinically discernible.
Other causes of lengthening of Quick's time and of activated partial thromboplastin time
Treatment with heparin
APTT is increased in patients undergoing heparin therapy. Lengthening of APTT depends on the type of heparin used, the circulating heparin concentration and the sampling time in relation to the time of heparin administration.
APTT results also depend on the sensitivity to heparin of the reagent being used. During haemostasis pre-surgery screening it is preferable to select a reagent relatively insensitive to circulating lupus anticoagulant.
Reagents used to determine Quick's time contain heparin inhibitor that renders them insensitive to heparin up to a specific circulating concentration of the latter substance.
Determination of thrombin time or assessment of anti-Xa activity may provide information about the presence of an anticoagulant such as heparin.
Presence of a specific inhibitor directed against a coagulation factor
Lengthening of Quick's time and of APTT occurs in the presence of a specific inhibitor directed against a coagulation factor to which one of these tests is sensitive. Presence of such an inhibitor is rare (other than in patients treated for haemophilia). Certain inhibitors, particularly specific inhibitors directed against factor VIII, result in exposure to extensive haemorrhagic risk. The clinical presentation may be pathognomonic and fortuitous detection during routine pre-surgery screening is rare.
Treatment with vitamin K antagonists
Treatment with vitamin K antagonists causes acquired deficiency in vitamin K-dependent coagulation factors (factors II, VII, IX and X), resulting in lengthening of Quick's time and of APTT. The degree of lengthening depends upon the sensitivity of the reagent to drug-induced deficiency in clotting factors, as does the extent of the resulting deficiency. This feature constitutes the reason for use of Quick's time, or preferably, its expression taking into account both the degree of the induced deficiency and of the sensitivity of the reagent, INR (International Normalized Ratio), for monitoring and adjustment of the vitamin K antagonist therapy.
Treatment with direct inhibitors
Treatment with direct thrombin inhibitors (argatroban, dabigatran, hirudin derivatives) results in lengthening of Quick's time and of APTT.
The degree of lengthening depends on the drug given and on the sensitivity of the reagent used, as well as the sampling time in relation to the time of drug administration. Determination of thrombin time may be used to identify the presence of a direct or indirect (heparin) thrombin inhibitor.
Treatment with direct activated factor X inhibitors
Treatment with direct inhibitors of activated factor X (rivaroxaban, apixaban) causes lengthening of Quick's time and of APTT. The degree of lengthening depends on the drug given and on the sensitivity of the reagent used, as well as the sampling time in relation to the time of drug administration. Determination of anti-Xa activity may be used to identify the presence of a direct or indirect inhibitor (heparin) of activated factor X.
